A single-center retrospective study compared the efficacy and safety of radiofrequency ablation against parathyroidectomy for secondary hyperparathyroidism in dialysis patients.
Abstract
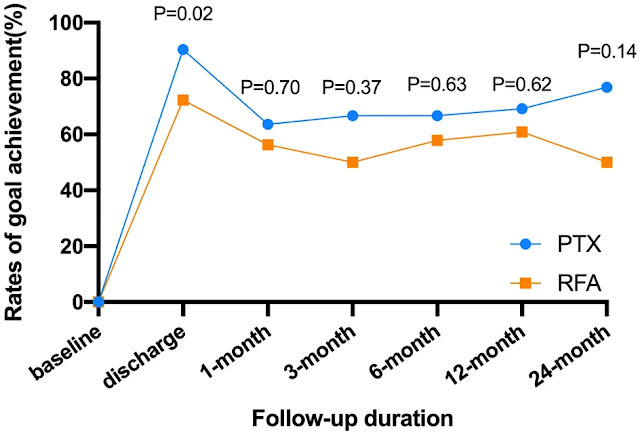
For the treatment of secondary hyperparathyroidism, we investigated the efficacy and safety of ultrasound-guided radiofrequency ablation (RFA) and parathyroidectomy (PTX) (SHPT). We separated patients into two groups in this single-center retrospective study: PTX (n = 53) and RFA (n = 47). The proportion of patients who achieved the target intact parathyroid hormone (iPTH) concentration range ( 300 pg/mL) was the primary outcome. Differential changes in iPTH, calcium, and phosphorus levels throughout time and prognosis were secondary outcomes. At the end of the study, iPTH values in the PTX and RFA groups were 82.1 percent and 64.1 percent, respectively, within the acceptable range (P = 0.07). After therapy, iPTH values in the PTX and RFA groups declined dramatically (82 163 pg/mL and 280 307 pg/mL, respectively, P 0.001). There was one.
There was no difference between the two groups in terms of iPTH, calcium, or phosphorus levels (P > 0.05). There were no differences in all-cause mortality or cumulative response rate between the two groups (P = 0.90 and P = 0.14, respectively) according to survival analyses. Notably, the RFA group had a reduced rate of infection and a shorter period of stay in the hospital. The pretreatment concentration of bone-specific alkaline phosphatase was linked to postoperative hypocalcemia. In the treatment of severe SHPT in maintenance dialysis patients, US-guided RFA is less intrusive than PTX and has been compared to PTX in terms of long-term efficacy and consequences. It could be utilised as an alternative to PTX; however, more research is needed.
Introduction
Chronic kidney disease (CKD) causes excessive release of parathyroid hormone (PTH), which causes secondary hyperplasia in parathyroid gland tissue and promotes a vicious cycle known as secondary hyperparathyroidism (SHPT)1. Resistance to fibroblast growth factor 23 (FGF23), which is caused by a malfunction of the FGF23-Klotho axis, is also a factor. SHPT is one of the main risk factors for death and cardiovascular events in patients with end-stage renal disease (ESRD)2. It causes bone pain and fractures, accelerates vascular calcification, lowers quality of life, and is one of the main risk factors for death and cardiovascular events in patients with ESRD.
Dietary restrictions, phosphate binders, and active vitamin D analogues such as calcitriol and newer calcimimetics3,4 are now used to treat SHPT. Due to adverse reactions or treatment resistance, active vitamin D compounds are useless for parathyroid hyperplastic nodules that have already formed. As a result, for severe drug-invalid SHPT, parathyroidectomy (PTX) is the usual treatment. 3,4. Any type of parathyroidectomy (total or subtotal) might result in long-term hypoparathyroidism and adynamic bone disease, necessitating calcium and calcitriol therapy.
Ultrasound (US) procedures such as microwave ablation (MWA)6,7 and radiofrequency ablation (RFA)8,9 of the parathyroid glands can be chosen for individuals with numerous problems who cannot tolerate PTX. Percutaneous ablation therapy guided by ultrasound is a minimally invasive, repeatable procedure that has been widely utilised to treat hyperparathyroidism. Previous research has shown that MWA or RFA can reduce PTH levels and are effective for SHPT10,11,12, and are not inferior to PTX in terms of safety and efficacy7,12,13,14,15; however, there are fewer comparisons between PTX and RFA in terms of hospital stay, economic costs, and especially long-term results.
Furthermore, "hungry bone syndrome"16 is caused by the quick consumption of calcium by bones as a result of the sudden decline in PTH following surgery. Convulsions, cardiac failure, seizures, and even sudden death can all be symptoms of severe hypocalcemia (SH)17. As a result, maintaining normal postoperative blood calcium levels is critical. Preoperative alkaline phosphatase (ALP)18 and PTH19 levels have been found to be independent risk factors for postoperative SH in patients with SHPT5,20 in a few investigations.
Clinical results, postoperative complications, and long-term prognosis of PTX and RFA in maintenance dialysis patients with SHPT were compared in this retrospective analysis.
Methods\sPatients
The Zhejiang Provincial People's Hospital's ethical and scientific review board gave its approval to this study. The retrospective cohort research included all patients diagnosed with SHPT who underwent PTX or US-guided RFA at our hospital from June 2014 to December 2020, and we confirmed that all techniques were executed in accordance with the applicable rules and laws of prophylactic declarations. (1) 18–85 years old; (2) dialysis vintage 6 months; (3) preoperative intact PTH (iPTH) concentration > 600 pg/mL; (4) severe SHPT after ineffective medical treatment; (5) at least one hyperplastic parathyroid nodules with diameter 1 cm found on US examination; and (6) follow-up durations 3 months were the inclusion criteria. (1) primary or tertiary hyperparathyroidism; (2) significant cardiopulmonary insufficiency were the exclusion criteria.
(3) a history of PTX or RFA; and (4) inadequacy and inability to tolerate therapy.
Intervention
For preoperative parathyroid localisation, all patients underwent regular high-frequency ultrasonography combined with 99mTc-sestamibi SPECT or enhanced CT. The doctor judged and fully described the two techniques to the patients based on the clinical guidelines and the patient's state. RFA is used by patients who cannot tolerate general anaesthesia or who desire minimally invasive treatment. They were divided into two groups based on their treatment: PTX and RFA.
The same clinician who had considerable expertise with US intervention and RFA treatment of parathyroid nodules conducted the US-guided RFA. Following cleaning and local anaesthetic, 10–30 ml of sterile water was injected around the parathyroid to create a heat insulation layer to protect neighbouring tissues from thermal harm. Grey-scale imaging was employed for guidance, while contrast-enhanced ultrasound (CEUS) with a high-frequency linear probe (L9-3) was used for monitoring, using an iU22 US scanner and a high-frequency linear probe (L12-5) (Philips, The Netherlands). To achieve thermal ablation, the needle of an 18G radiofrequency electrode (VIVA; STARmed, Goyang, Korea) with a 7 mm active tip was introduced into the target parathyroid nodules. During the procedure, the doctor assessed the patient's health.
If hoarseness developed, the surgeon quickly stopped the procedure. We kept a watchful eye on whether hematoma or hypoxia developed during postoperative care. Patients eventually resumed eating after 4 hours. We checked whether the patients had hoarseness or bucking on a regular basis. If the degree of iPTH drop was unacceptable, more testing was required to identify whether a residual or ectopic parathyroid gland existed.
After general anaesthesia and normal cleaning, whole PTX was given. In a supine position, the patient was placed. The dermatoglyphic direction of the anterior transverse neck incision was approximately 5 cm. The skin flaps were split and secured beneath the skin flaps.
Along the white line of the neck, the platysma and anterior cervical muscles were separated. The surgeon carefully separated and preserved the bilateral recurrent laryngeal nerves after thoroughly exposing the thyroid and parathyroid glands, and then totally removed all visible parathyroid glands. The anterior neck incision was sutured layer by layer after complete hemostasis. The procedure involved cutting around 30–60 mg of parathyroid tissue into 1 1 1 mm particles and implanting them on the forearm brachioradialis.
Obtaining clinical data
Age, gender, dialysis history, clinical symptoms, and treatment protocols were all gathered. Baseline clinical laboratory variables such as serum creatinine (Cr), uric acid (UA), albumin (ALB), haemoglobin (Hb), troponin I (TNI), B-type natriuretic peptide (BNP), C-reactive protein (CRP), iPTH, calcium (Ca), and phosphorus (P) levels, as well as bone metabolism-related indicators such as bone-specific alkaline phosphatase (bALP), The number and size of parathyroid nodules, osteoporosis (bone density), carotid arteriosclerosis (carotid artery B-US), hospital stay, and postoperative complications were all factors considered in the study.
Results and follow-up
1-month (2 weeks), 3-month (2 weeks), 6-month (1 month), 12-month (1 month), and 24-month (1 month) serum iPTH, calcium, and phosphorus concentrations were measured after PTX or RFA at the following time points: 1-month (2 weeks), 3-month (2 weeks), 6-month (1 month), 12-month (1 month), and 24-month (1 month). All patients were tracked until death, kidney transplantation, loss, or the study's conclusion (June 30, 2021).
During the efficacy assessment phase, the proportion of patients in the PTX or RFA groups having an iPTH concentration in the target range was the primary outcome (follow-up to the endpoint).
The target range of iPTH concentration was maintained at approximately 2 to 9 times the upper limit of normal, according to the Kidney Disease Improving Global Outcomes (KDIGO) Guidelines21, with goal achievement for iPTH of 124–558 pg/mL, calcium of 2.0–2.5 mmol/L, and phosphorus of 0.97–1.62 mmol/L. The lowest iPTH level following a successful surgery within 7 days was less than 300 pg/mL, according to prior research and guidelines19,21,22. As a result, our research determined that the postoperative iPTH level should be fewer than 300 pg/mL.
Differences in iPTH, Ca, and P levels throughout time between the two groups, long-term prognosis (death or recurrence), and the occurrence of postoperative adverse events were the secondary endpoints (hoarseness, fever, hematoma, and hypocalcemia). The
The cumulative response rate was defined as the percentage of patients who had an iPTH level of less than 558 pg/mL for three months before the end of the research while their preoperative clinical symptoms were entirely gone. A serum iPTH value of more than 558 pg/mL was considered as recurrence. In clinical practise, serum Ca less than 2.0 mmol/L was called hypocalcemia, and serum Ca less than 1.8 mmol/L was deemed SH, requiring intravenous Ca5,17. Oral calcium carbonate (1.8–5.4 g/day) and calcitriol (1.0–2.5 g/day) were provided if blood Ca was between 1.8–2.1 mmol/L during the perioperative period.
Analytical statistics
SPSS version 26.0 for Mac Sciences version 9.0 was used for all statistical studies. The mean and standard deviation (SD) of the measured data adhering to a normal distribution are displayed, while the median and interquartile range are displayed for the other data. The independent sample t test, Mann–Whitney U test, or chi-squared test were used to make comparisons between parameters. During the efficacy assessment phase, a linear mixed model was employed to compare serum iPTH, Ca, and P concentrations between the groups. Logistic regression analysis was used to look at potential hypocalcemia predictors. The Kaplan–Meier survival curves were used to calculate the survival analysis. All of the findings were put to the test using bilateral testing, with a significance level of P 0.05.
Ethical Statement
The Zhejiang Provincial People's Hospital's ethical and scientific review board examined and approved this study protocol, with approval number [2021QT330]. In addition, the study has been exempted from the requirement of written informed consent.
Results
Information in general
Between June 2014 and December 2020, a total of 100 individuals received treatment. There were 53 patients in the PTX group, with 47 (88.7%) receiving total PTX with AT and 6 (11.3%) receiving entire PTX; there were also 47 patients in the RFA group, with 26 (55.0%) receiving single-session RFA and 21 (45%) receiving two-session RFA.
Table 1 summarises the baseline characteristics of the patients. The patients were 51 and a half years old on average. The average vintage of dialysis was 7.8 3.6 years. The median follow-up period was 30.025 (22.325–38.725) months, with hemodialysis being used by 81 percent of patients. In various variables, such as age, sex, dialysis history, follow-up time, renal function, UA, ALB, Hb, CRP, TNI, BNP, iPTH, calcium, phosphorus, and bALP (P > 0.05), there were no statistical differences between the two groups.
The PTX group had more parathyroid hyperplasia nodules; 3.9 0.4 lesions were resected in the PTX group versus 3.68 0.63 nodules ablated in the RFA group (P = 0.03). The greatest nodule diameter and preoperative clinical complaints (ostealgia or arthralgia, cutaneous pruritus, skeleton distortion, and calcinosis cutis) did not differ significantly between the two groups. The presence of chronic kidney disease-related mineral and bone disorder (CKD-MBD) in both groups was suggested by the results for bone-derived turnover markers, osteoporosis, and vascular calcification.
Primary outcomes are those that occur as a result of the actions taken.
90.4 percent and 72.3 percent of patients in the PTX and RFA groups, respectively, had iPTH concentrations within the goal range ( 300 pg/mL) at the time of discharge (P = 0.02, Table 2). At all of the follow-up dates, however, there were no significant differences in the rates of iPTH goal attainment between the two groups (Fig. 1). Furthermore, at the study's endpoint, iPTH values of 82.1 percent and 64.1 percent in the PTX and RFA groups, respectively, met the suggested goal (P = 0.07). Individuals in the PTX group showed considerably lower iPTH readings (50 pg/mL) than those in the RFA group (38.7% vs. 2.6 percent, P 0.001), and these patients may have had irreversible hypoparathyroidism.









No comments:
Post a Comment